Our bodies are made up of countless living cells and we have genes that manage, or control, normal cell growth, division and death. This process is really rapid when we’re young to allow us to grow. As we get older, cell division mostly occurs to replace dying cells or to repair injuries.
When this normal cell cycle is disrupted for any reason, the old cells do not die but continue to grow and multiply into abnormal cells. Cancer cell growth is different from normal cell growth in that it is not regulated and cannot be controlled by normal checkpoints in the body that work on normal tissues. Sometimes these abnormal cells overrun normal tissues or invade surrounding brain structures.
A tumor forms when these abnormal cells grow, sometimes very rapidly, into an abnormal mass of tissue. The tumor can compress, shift or replace normal tissue, sometimes, but not always leading to signs and symptoms that lead you to seek medical attention. Sometimes tumors are discovered during the course of other medical examinations.
Tumors that form from the tissues of the spine are called primary tumors. These tumors can be either malignant or benign. A tumor that is benign is usually less aggressive and slower growing, but can become just as serious as a malignant tumor, and even life threatening, if it interferes with spine function. Primary tumors originate from cells that make up the spine and central nervous system and are usually named for those cells.
The underlying cause of primary spinal tumors remains largely unknown. Some tumors may grow due to exposure to cancer-causing agents and some may be attributed to a compromised immune system. There is also the possibility of a genetic component to the growth of spinal tumors.
A fraction of spinal tumor diagnoses are caused by rare genetic diseases such as neurofibromatosis 2 and Von Hippel-Lindau disease. Research is ongoing into genetic and environmental factors that may contribute to the development of spine tumors. Age is considered a risk factor as well, with older people being diagnosed at a much higher rate than younger people.
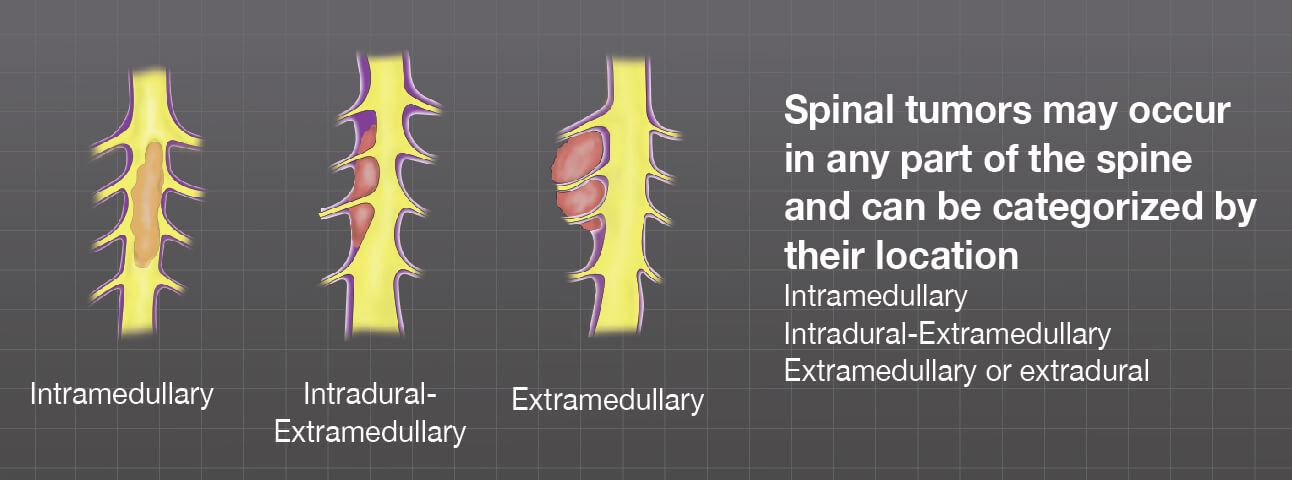
Spine tumors may be referred to by one of the main structures of the spine including cervical (neck), thoracic (upper back), lumbar (lower back) and sacral (tailbone). They may also be categorized by the part of the spine in which they form.
Intramedullary
These tumors grow inside the spinal cord itself.
Intradural-extramedullary
Tumors that grow outside of the actual spinal cord but inside the dura mater, or outermost layer of the spinal cord covering
Extramedullary or extradural
These tumors grow outside of the dura mater or outermost layer of the meninges, which is also called the spinal cord covering. Most of the time these tumors are metastatic but may be primary to the bone.
Physiologically, you may not know you have a brain tumor. Visit our Investigate Spine Tumors section of the website to explore the Signs, Symptoms and Diagnosis of Spine Tumors more in depth.